A research group from the Ludwig Boltzmann Institute for Experimental and Clinical Traumatology has determined how levels of microRNA in the bone and blood change within an animal model of postmenopausal osteoporosis.
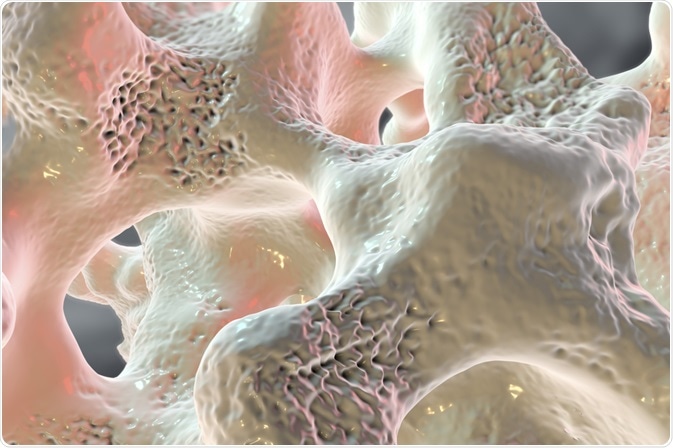 Image Credits: Kateryna Kon / Shutterstock.com
Image Credits: Kateryna Kon / Shutterstock.com
The present study is part of the “TAMIBAT-Project” (Time-dependent Analysis of microRNAs and Bone Microstructure under Consideration of Anti-Osteoporotic Treatment) which investigates the role of anti-osteoporotic treatment on bone-related miRNAs in bone tissue and serum.
The team found that osteoanabolic and anti-resorptive therapy was found to increase microRNA transcription in bone tissue in ovariectomized rats (OVX). The corresponding changes in the microRNA levels in placebo-treated OVX rats were reverted by anti-osteoporotic therapy. The microRNA miR-203a was found to be up-regulated by OVX treatment and down-regulated following therapy. Moreover, the correlation between bone and serum levels of miR-203a is significant.
miRNAs offer clinical utility as biomarkers and drug targets for bone disease as they exert influence on the genes that control bone metabolism. To investigate their role, an animal model of postmenopausal osteoporosis was used to generate data reporting in the regulation of miRNA in bone and peripheral blood throughout periods of bone loss and during preventative treatment.
This included osteoanabolic treatment, which describes therapy intended to increase bone mass and anti-resorptive therapy slows or prevents the resorption of bone. The latter serves to restore skeletal balance as bone turnover is reduced.
Laboratory rats were assigned sham surgery or an ovariectomy; sham surgery refers to a ‘faked’ surgery which mimics the same steps of the ‘real’ surgical intervention without performing the restorative step, presumed to have therapeutic benefit. Eight weeks following surgery, the OVX rats underwent further randomization.
The two groups were subject to treatment with two classes of bisphosphonates; osteoanabolic treatment or an anabolic bone-promoting agent. Following 12 weeks of treatment, bone and serum samples were subject to microRNA analysis using next-generation sequencing (NGS). mRNA levels using RT-qPCR and the bone microarchitecture was analyzed using nanoCT.
Kocijan et al. found that the microRNA levels in rodent bone tissue and cell-free blood (serum) during a period of bone loss induced by hormones and in response to anti-resorptive and anabolic bone loss.
There was a reduction in trabecular bone 20 weeks following treatment in ovariectomized and untreated animals. Treatment with an anabolic resulted in bone loss rescue, and the anti-resorptive treatments achieved only partial rescue. Similar results were found at the vertebral and tibial sites.
Femoral head tissue is amenable to quick and reproducible analysis. This site was used to obtain bone miRNA levels. Without therapy, ovariectomized rats represent the postmenopausal osteoporotic state. Distinct microRNA signatures were found in untreated OVX animals relative to ani-resorptive and anabolic treated animals.
A total of 11 miRNAs were upregulated in the untreated OVX group and downregulated in both treatment groups. These miRNAs are mechanistically relevant in the guarding of postmenopausal bone loss. However, mtRNA expression of SHAM and treated animals were comparable.
The second major finding by Kocijan and colleagues was the upregulation of miR-203a expression in ovariectomized untreated rats and subsequently rescued by treatment. These levels of miR-203a were also significantly correlated with levels in bone. This miRNA is implicated in bone formation and mesenchymal stem cell differentiation; particularly osteoblasts, which is caused by osteogenic effectors up-regulated by miR-203a.
miR-203a additionally inhibits a regulator (Dlx5) of the transcription factors RUNX2 and Osx, that are involved in bone formation. Inhibition of Dlx5 results in transcription factor inhibition; in their absence, mesenchymal stem cell differentiation is prevented. The sum effect is slowing of osteoblastic differentiation and therefore encourages bone loss development.
The team as surprised to discover the downregulation of Dlx5 and Runx2 with the treatment of the anabolic agent; despite the increase in bone microstructure and density. However, Runx2 concentration is thought to oscillate, indicating the time of analysis is pertinent. Moreover, RNA and protein levels are not necessarily correlated; the action of anabolic agents is complex, and while miR-203a is a regulator of osteoblast differentiation, it is not representative of the whole-body microenvironment.
The finding that miR-203a levels in serum and bone are correlated indicate tight regulation and the appropriateness of biopsies in the in miRNA detection. In addition, miRNAs have demonstrable clinical utility as biomarkers as changes in their expression have been corroborated in other experiments.
The team found changes in an additional miRNA, miRNA-133, an inhibitory transcription factor in bone formation. Downregulation of miRNA-133 suggested that bisphosphonates exert a positive effect on bone formation, through the action of Runx2
This study represents the first miRNA study in postmenopausal osteoporosis treated by bisphosphonates. Notable effects were seen on the regulation of miRNA expression in the bone in response to hormone-induced bone loss. Osteoanabolic and anti-resorptive treatment represented a therapeutic intervention that could restore miRNA levels. Thus the team successfully demonstrated the clinical utility of bone-derived miRNAs as a minimally-invasive biomarker.
Funding
This study was supported by the FFG Feasibility Project Grant 852770, the Christian Doppler Gesellschaft, EU-FP7 Health Project FRAILOMIC305483and EU-FP7 Health Project SYBIL602300.
Source
Kocijan, R. et al. (2020) MicroRNA levels in bone and blood change during bisphosphonate and teriparatide therapy in an animal model of postmenopausal osteoporosis. Bone. doi: https://doi.org/10.1016/j.bone.2019.115104
Further Reading