The cardiovascular system can be monitored and its functionality assessed with cardiovascular magnetic resonance (CMR) imaging. New techniques for CMR imaging have been developed in recent years. These include T1 and T2 image mapping, which are non-invasive imaging techniques that have been quickly integrated into normal CMR imaging procedures.
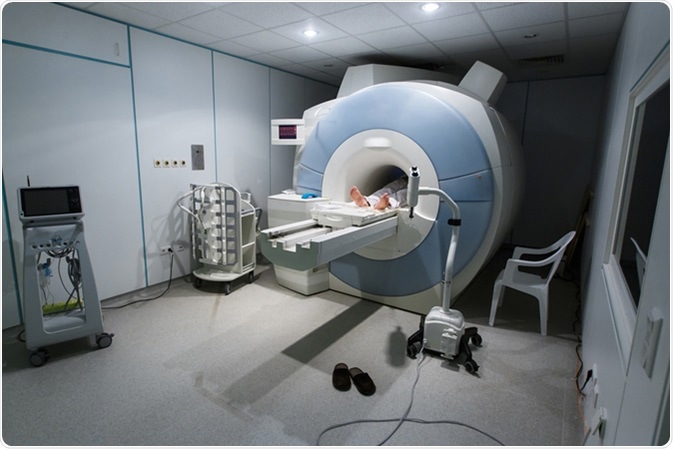
MRI (magnetic resonance imaging) scanner in a hospital. Image Credit: zlikovec / Shutterstock
Although many diseases affecting the heart muscle do not produce changes in signal intensity, motion, or enhancement on normal MRI scans, they may affect myocardial nuclear magnetic resonance (NMR) properties, including T1 and T2 relaxation times. Estimates of relaxation times can be produced using pulse sequences optimized for cardiac imaging.
Indications for Cardiac Magnetic Resonance Imaging
What is T1 mapping?
T1 is another term for spin-lattice relaxation time. It is a measurement of how quickly the net magnetization factor (NMV) returns to its thermodynamic equilibrium along the B0 direction. The majority of myocardial disorders result in prolonged myocardial T1; however, T1 is sometimes shortened in patients with Fabry disease, hemochromatosis, fatty arrhythmogenic right ventricular dysplasia (ARVD), and also due to gadolinium contrast accumulation, which will shorten T1 in both diseased and healthy heart muscle. However, contrast agents like gadolinium aren’t always necessary for T1 mapping, to the advantage of the patient.
The most commonly used T1 measuring method uses only two to three inversion pulses, and is called Modified Look-Locker Imaging (MOLLI). The inversion pulses are followed by several single-shot-b-SSFP readouts. Longitudinal magnetization between cycles is recovered during rest periods between cycles that are factored into the measurement. This method is able to generate accurate myocardial T1 measurements in one breath hold, or approximately 20 seconds. Shortened MOLLI (shMOLLI) is used for patients who cannot hold their breath for 20 seconds or more, requiring only nine heartbeats as opposed to 17. When imaging does use gadolinium contrast dye the recovery period can be shortened, as gadolinium myocardium will produce lower T1 values.
An advantage of T1 mapping is that it can identify abnormalities in the myocardial system immediately. Another advantage is that it is able to produce quantitative assessments of abnormalities in the heart’s muscular system. Both T1 and T2 mapping use parametric quantitative sequences, allowing doctors to gain T1 and T2 values for specific tissues. It is also possible to produce color-encoded T1 maps to identify very small T1 variations, mirroring abnormalities in the heart muscle. Extracellular volume (ECV) measurement is also possible with T1 mapping, offering a non-invasive alternative to myocardial biopsies.
What is T2 mapping?
T2 is another term for spin-spin relaxation, or transverse relaxation time. Like T1, it is a biological parameter of CMR imaging that is used to identify abnormal myocardial tissues through tissue-specific time parameters. T2 mapping is carried out using a balanced steady-state free precession (SSFP) readout after a multinomial T2-preparation module. T2 values can, like T1 values, be measured from a color-encoded map.
There are two types of T2 mapping techniques. The first type is dark-blood turbo spin-echo (TSE), and the second type is bright-blood T2-preparation pulse-based sequences. T2 mapping using TSE is susceptible to some restrictions: for instance, loss of signal may be experienced due to artifacts from blood flow that increase the appearance of bright subendocardial rims from stagnant blood, and through-plane motion. Loss of signal can also be experienced from the posterior wall because of cardiac movement. Conversely, T2-preparation-based imaging techniques are not as sensitive to artifacts linked to TSE.
While longer T1 values are attributed to many abnormalities, longer T2 relaxation times are attributed to higher water content in myocardial tissue. T2 is very useful for highlighting myocardial edema in patients with acute myocardial infarction (AMI), myocarditis, stress cardiomyopathy, sarcoidosis, and cardiac allograft rejection.
In addition to the detection of and predictions about myocardial abnormalities , T2 mapping can also be used to detect early breakdown of articular cartilage. As such, quantitative T2 can be used as a biomarker for osteoarthritis. It highlights the interaction of increased water content and the extracellular matrix, and can also help to predict the way in which cartilage degeneration will progress. T2 mapping can be used to assess repair tissues, and it also has the advantage of being able to produce high-resolution 3D images in a short amount of time, increasing its clinical potential.
Further Reading