The immune system can be divided into two types of responses; innate and adaptive immunity. The innate immune system is present from birth and does not exhibit any immunological memory, whereas the adaptive immune system remembers pathogens upon future encounters.
 Credit: Katryna Kon/Shutterstock.com
Credit: Katryna Kon/Shutterstock.com
The adaptive immune system is slow to respond to a pathogen on its first exposure. The innate immune system is a much faster response system that operates on the cellular level in the early hours and days of an exposure.
Innate immune responses are generalized, rather than specific to a particular pathogen. The adaptive immune system evolved relatively recently and is specific to vertebrates, whereas innate immunity is older and is also found in invertebrates and plants.
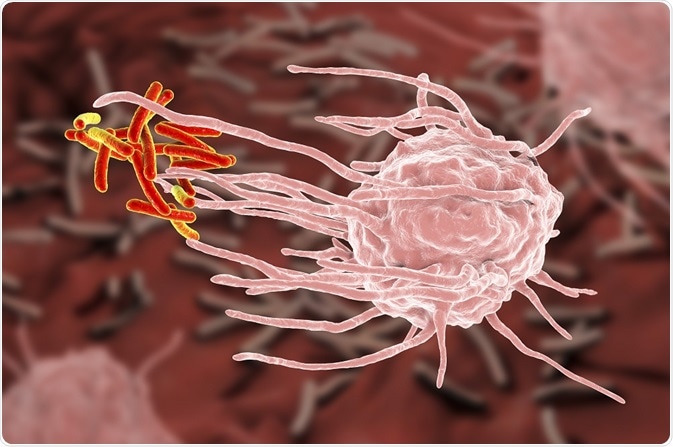
Every cell can activate an innate immune response. However, macrophages and other phagocytes have additional roles that make them are crucially important to the innate immune system.
How the innate immune response works
The immune system must be able to distinguish self from non-self and self in order to initiate an immune response. This ability is based on recognition of molecules, called pathogen-associated immunostimulants that are common in pathogens but not present in the host. These molecules trigger inflammatory responses and phagocytosis.
Pathogen-associated immunostimulants include molecules like formylated methionine that are specific to prokaryotic organisms, as well as molecules commonly associated with microorganisms.
Examples include:
- Peptidoglycan cell walls
- Bacterial flagella
- Lipopolysaccharides (present on gram-negative bacteria)
- Teichoic acids (present on gram-positive bacteria)
- Fungal proteins including zymosan, glucan, and chitin
- Parasitic membrane components such as glycosylphosphatidylinositol in plasmodium
- Short nucleic acid sequences from bacteria
Cells also have pattern recognition receptors (PRRs) that can detect repeating patterns of pathogen-associated immunostimulants on the surface of the organism. They recognise molecules called pathogen-associated molecular patterns on the surface of bacteria and other organisms.
Examples of pattern recognition receptors include some members of the complement system and membrane-bound receptors on the host cell surface, such as Toll-like receptor family. Those receptors can then initiate phagocytosis of the pathogen and stimulate expression of genes in the host cell that are involved in the innate immune response.
Specific cells of the innate immune response
Macrophages and neutrophils are phagocytic cells that engulf a microbial pathogen after it has been identified by the innate immune system. Macrophages are cells that are present in vertebrates in tissues throughout the body, particularly those vulnerable to infection, like the lungs and gut.
Macrophages are long-lived cells that monitor tissues and offer the earliest response to an invasion. Neutrophils are shorter-lived cells that are present in the blood, but not in normal tissue. They are recruited to sites of infection by macrophages and by the microbes themselves through the release of peptides containing formylmethionine.
Macrophages and neutrophils use receptors on their cell surfaces to recognize and engulf pathogens, as well as receptors for antibodies produced by the adaptive immune system and for the C3b component of the complement system. If a ligand binds to any of these cell surface receptors, the cell’s membrane begins to surround the pathogen and ultimately encloses it in a phagosome.
Once the pathogen is inside the phagosome, it is destroyed through acidification, merged with a lysosome, and degraded by lysozyme and hydrolases that break down the cell walls and proteins. The NADPH oxidase complex produces toxic oxygen-derived compounds like superoxide, hypochlorite, and nitric oxide that increase the oxygen consumption of the cells.
Macrophages typically survive this process. However, neutrophils are usually killed with the cells that they destroy. These neutrophils largely comprise pus produced by infected wounds, whose greenish color is attributable to an enzyme, myeloperoxidase, which contains copper.
Pathogens too large to be phagocytosed will be consumed by a group of immune cells that gather around it. They secrete toxic products to induce the same process that would normally occur inside the phagosome.
Further Reading